Fertility benefits for IVF may provide financial coverage for treatments and procedures as well as other support including care navigation and educational resources. While comprehensive fertility benefits can significantly reduce the financial burden of fertility treatments, not all employers offer this coverage.
What is IVF:
In vitro fertilization (IVF) refers to a series of different processes that can help a person become pregnant.
IVF is the most effective type of assisted reproductive technology (ART) and incorporates the use of various medications and procedures that help a sperm cell fertilize an egg cell to produce an embryo and to help the embryo implant in the uterus.
During IVF, medications are used to stimulate multiple eggs to grow to maturity inside the ovaries.
These eggs are then retrieved from the ovaries during a minor medical procedure and fertilized by sperm in a laboratory.
A thin needle is inserted through the vaginal wall and the collected eggs are fertilized with sperm from the partner or sperm donor.
The fertilized eggs, now embryos, are cultured in a controlled environment in the laboratory.
They are monitored for growth and development over the next few days.
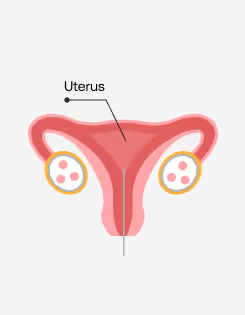
The embryo is then transferred to the uterus.
This process can take about three weeks from start to finish if the full IVF cycle is done all at once. In some cases, people going through IVF may split the process up into different steps, which can make the process take longer.
People may go through IVF for a variety of different reasons, but it is often used to treat infertility in women over 40. IVF may also be an option for individuals with certain health conditions such as endometriosis, uterine fibroids, ovulation problems, fallopian tube issues, and more. If the fallopian tubes are blocked or damaged, getting pregnant without medical help may be difficult or impossible. IVF bypasses the need for fallopian tubes by allowing fertilization to occur outside the body.
The history of IVF dates back to the 1960s and 1970s, when scientists started exploring the possibility of fertilizing human eggs outside the body, often in a test tube or culture dish in a laboratory setting.
.webp)
During the 1970s, significant progress was made in refining the techniques for human IVF. The first "test-tube baby” was born in England in 1978, and three years later, the first IVF baby was born in the U.S.
The IVF process has evolved considerably since its inception and today accounts for about 1–3% of all annual births in the U.S. and Europe.
Who are candidates for IVF?
There are many different types of people who may consider IVF.
Infertility is defined as being unable to achieve pregnancy within 12 months of unprotected intercourse or therapeutic donor insemination for those younger than 35 years or within 6 months for those older than 35 years. Up to 15% of couples are diagnosed with infertility. A variety of factors can cause infertility in both males and females. While some causes may be treated with medical interventions or lifestyle modifications, some individuals or families experiencing infertility may need a form of ART such as intrauterine insemination (IUI) or IVF in order to get pregnant.
Some people opt for IVF in order to reduce the risk of passing along hereditary disorders to their children. There is a laboratory procedure often performed in conjunction with IVF called pre-implantation genetic testing for monogenic/single gene disorders PGT-M, which can lower the risk of passing along inherited single gene conditions such as sickle cell anemia and cystic fibrosis.
IVF may be an option for individuals preparing to receive cancer treatments or other medical treatments that can affect fertility. Many experts recommend freezing embryos or eggs, prior to cancer treatments because some surgeries and treatments can cause permanent fertility changes.
For same-sex couples, IVF may be an effective way to form a family. A type of IVF known as reciprocal IVF can be an option for lesbian or trans couples who want to build their family. Reciprocal IVF involves one partner contributing eggs to form an embryo and one partner receiving the embryo and carrying the pregnancy. Same-sex cisgender male couples may choose to go through gestational surrogacy (GS) and use a gestational carrier (GC). This means a person is hired as a GC to carry and give birth to a baby for another person or couple.
A single parent by choice is someone who chooses to have a child knowing they will be that child’s sole provider, at least at the beginning. People may choose this path for different reasons, and donor-assisted reproduction is one way to make single parenthood possible. In this form of ART, donated eggs, embryos, or sperm are used to give single parents the option to have genetically related children independently.
How to prepare
for IVF
There are many physical, emotional, and logistical considerations that go into preparing for IVF.
In addition to a comprehensive medical evaluation that includes an examination of both partners' reproductive health and hormone levels, and a genetic screening, the preparation process may also include lifestyle modifications such as the incorporation of a balanced diet and regular exercise, and the avoidance of tobacco, excessive alcohol, and other harmful substances.
- Because of the potential emotional toll IVF can take, many experts also recommend that individuals or couples preparing for the process consider counseling and support groups to help cope with stress and anxiety.
- Financial planning is also a necessary step for many people preparing for IVF as the process can be costly in the absence of a comprehensive fertility benefits package.
- Finally, advanced scheduling is an important part of the IVF journey as the process requires regular appointments, medication administration, and a medical procedure.
Selecting an IVF clinic is a crucial decision, as it can significantly impact the chances of success and the overall experience. Here are some important factors to consider when choosing an IVF clinic:
Success rates: Patients should look for clinics with a track record of successful pregnancies
Accreditations and certifications: Patients should ensure the clinic is accredited by relevant medical associations and regulatory bodies in their country.
Experience and expertise: Patients should research the clinic's medical team including their specialization in reproductive medicine, and any advanced training they might have.
Technology and facilities: Modern, well-equipped facilities contribute to better outcomes.
Services offered: In addition to IVF, clinics may offer a range of services like egg freezing, embryo freezing, preimplantation genetic testing (PGT), and more.
Personalized care: It’s important to find a clinic that provides personalized treatment tailored to each patient’s specific needs.
Patient reviews and testimonials: Patients should read reviews and testimonials from others who have undergone treatment at the clinic and can offer insight into their experience.
The first step in seeking fertility guidance and care is to schedule an initial consultation and health evaluation with a fertility specialist or reproductive endocrinologist.
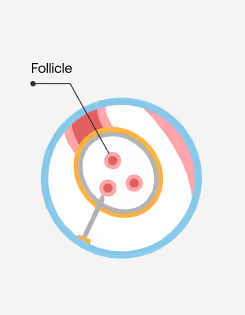
A transvaginal/pelvic ultrasound is an imaging procedure that visualizes the cervix, uterus, fallopian tubes, and ovaries. During a transvaginal/pelvic ultrasound, a provider will gently insert a wand-like instrument called a transducer into the vagina to record images of the pelvic organs. This can help identify any abnormal structures or growths and during IVF, this same procedure is used to monitor the development of the follicles inside the ovaries.
AFC is a key tool used to assess the ovarian reserve (number of remaining eggs) and potential fertility. AFC is typically measured during transvaginal ultrasound during the early phase of the menstrual cycle.
AMH is produced by the ovaries and is considered a potentially important indicator of reproductive health. An AMH test measures the amount of AMH in a blood sample and correlates with the number of eggs in the ovaries; higher levels of AMH typically means the ovaries have a larger supply of eggs. With age, the number of eggs decreases, causing AMH to also decrease; at menopause, AMH levels drop to zero when there are no eggs remaining in the ovaries.
In addition to an AMH test, other common blood tests can help provide insight into a woman’s ovarian reserve (i.e., the number of eggs available for potential fertilization). The most common hormones to test before IVF include follicle FSH, which is considered a predictor of reproductive aging, LH, which can indicate egg quality, and estradiol (often referred to as E2), which, in combination with the other tests, can offer insight into other factors of fertility.
Once the provider receives all the test results and data, they will schedule a time to discuss findings, any potential causes of infertility, and available treatment options, which may include IVF.
The cost of IVF
The cost of IVF can vary significantly depending on several factors, including geographic location, the prescribed treatment plan, the specific clinic, and any additional procedures or tests required.
The average cost of one cycle of IVF in the U.S. can range from $12,000 to $15,000, but these prices do not include the cost of necessary medications or other services such as genetic testing and embryo freezing.

While IVF costs vary widely, the total expense of a single cycle can typically be broken down to reflect the following components:
Initial consultation and diagnostic tests: This usually includes the first appointment with the fertility specialist or reproductive endocrinologist, medical history review, physical exams, blood tests, ultrasounds, and semen analysis.
Medications: The IVF process requires a variety of medications to stimulate the ovaries, control the menstrual cycle, and prepare the body for embryo transfer. Costs of these medications vary widely depending on a number of factors but medication expenses can often comprise a significant percentage of the total cost of IVF.
Egg retrieval: Retrieving the mature eggs from the ovaries requires a surgical procedure, often including an additional cost for anesthesia.
Sperm collection: If necessary, a medical provider may order sperm tests in order to analyze the sperm and prepare for fertilization.
Insemination or intracytoplasmic sperm injection (ICSI): In some cases, fertility specialists may recommend using a specific laboratory method to fertilize the eggs with sperm.
Embryo culture: Once the eggs are fertilized with sperm, the resulting embryos require several days of monitoring and culturing in a laboratory.
Embryo transfer: If the embryos are being transferred immediately following the retrieval and culturing, there will be a cost to cover the procedure to implant the embryo into the uterus.
Optional cryopreservation: If the embryos are not being transferred immediately, there will be a cost for freezing and storing the embryos for future use.
Optional genetic testing: In some cases, a provider may recommend preimplantation genetic testing (PGT) to screen embryos for genetic abnormalities.
Additional procedures: If necessary, an IVF cycle may require additional procedures like assisted hatching or embryo biopsy at extra costs.
Insurance coverage of IVF varies significantly depending on the country, state, and specific insurance plan. But in many other countries, including the U.S., most insurance plans do not offer comprehensive coverage for IVF. Some insurance plans may offer partial coverage for specific parts of the IVF process, like diagnostic testing or medications. These plans often do not cover the entire IVF process, however, and many other plans do not offer any IVF coverage at all, leaving individuals or couples to pay for the full cost of treatment out-of-pocket. The high cost of treatment and limited insurance coverage for IVF create significant barriers to access for many people, which can make it challenging to pursue fertility treatments without incurring substantial financial burdens or debt.
For individuals or couples seeking financial assistance, there are several financing options available for IVF.
Some fertility clinics offer financing programs or partnerships with financial institutions, providing loans or payment plans tailored to cover IVF expenses.
Some credit card companies offer medical credit cards that can be used to pay for medical procedures, including fertility treatments like IVF. These cards often come with promotional financing options, such as interest-free periods.
There are several non-profit organizations and foundations dedicated to providing fertility grants and scholarships to individuals and couples with financial need who are pursuing fertility treatments.
Some insurance plans offer partial coverage or FSAs (pre-tax dollars) that can be used for fertility treatments like IVF.
Employers that offer comprehensive fertility benefits such as Carrot can help employees save money with reimbursement options and provide a simplified payment method for fertility and family-forming care in the form of the Carrot Card.
An increasing number of employers are offering fertility benefits to workers seeking treatments such as IVF. These benefits are designed to support employees facing fertility challenges, interested in fertility preservation, or exploring other family-forming options.

Before beginning an IVF journey, it’s important to check an employer’s fertility benefit offerings by reviewing an employee handbook, specific health insurance policy documentation, or speaking with a representative in human resources (HR). If an individual’s company does not offer fertility benefits, it may be helpful to attend benefits enrollment meetings to ask questions about fertility coverage in the future.

If you don't have fertility benefits at your company, Carrot can reach out on your behalf.
The IVF process step-by-step
The IVF journey is individualized for a variety of reasons, but in general, the process includes several steps to stimulate egg production and maturation, and fertilize eggs and sperm outside the body in a laboratory setting to create embryos. If the IVF process results in one or more healthy embryos, those embryos can then be frozen for future use or transferred into the uterus for potential implantation.

Success rates of IVF
According to the Society for Assisted Reproductive Technology, age is the most important factor when determining success rates of all ART methods.
Success rates decline as women age and this decline becomes more drastic after a woman reaches her mid-30s. This decline in success is influenced by the decreased chance of getting pregnant through ART in combination with the high rate of miscarriage with age, particularly over age 40.
The number of live births per intended egg retrieval (embryo transfers) in 2020 demonstrates the success rates of IVF at various ages.
The Centers for Disease Control and Prevention (CDC) reports that there were 326,468 ART cycles performed at 449 reporting US clinics during 2020, resulting in 75,023 live births ( one or more living infants delivered) and 79,942 live born infants. Of that total number of cycles performed in 2020, 123,304 were egg or embryo banking cycles in which all resulting eggs or embryos were frozen for future use. The CDC estimates that about 2% of all infants born in the US every year are conceived using ART.
.svg)
There are many factors aside from age that can also affect success rates of IVF. Low or high weight or body mass index (BMI), smoking, alcohol use, diet, vitamins, supplements, and stress can all take a toll on the likelihood of success with IVF. There are many potential lifestyle factors that may help improve the success rate of IVF, so patients are advised to work closely with their fertility providers to find well balanced food and exercise plans that work for them, as well as reducing or quitting alcohol, tobacco, and other substances.
Fertility experts often also recommend specific supplements and vitamins prior to and during IVF to help optimize fertility. Because sperm and egg cells take about 90 days to develop, it may be important to start taking vitamins and supplements in the months prior to IVF. Prenatal vitamins can help support egg quality and ovarian reserve, as well as the development of the uterine lining, and other aspects of fertility and overall health. It is important for prenatal vitamins to contain folate, a form of vitamin B-9.
The risks and side effects of IVF
Like all medical interventions and procedures, there can be some risks and side effects associated with the IVF process
The medications involved in IVF carry risks of side effects including:
Hot flashes
Mood swings
Irritability
Breast tenderness
Headaches
Abdominal discomfort
Restlessness
Ovarian hyperstimulation syndrome (OHSS)
Fatigue
OHSS is a medical condition that can occur as a result of the medications used during fertility treatments, particularly IVF. It involves an exaggerated response of the ovaries to the hormonal stimulation used to induce the development of multiple follicles (fluid filled sacs containing eggs). When OHSS develops, the ovaries swell and fluid accumulates in the abdominal and sometimes chest cavities. Symptoms of OHSS include: abdominal discomfort or pain, weight gain, nausea, vomiting, shortness of breath, decreased urination, increased heart rate and blood pressure. Severe OHSS is rare and can be dangerous. Prevention and management are important considerations in fertility treatment and your healthcare team will closely monitor your response to medications to ensure your safety and well-being throughout the process.

Other risks of IVF include the chance of multiple births, which can occur if more than one embryo is transferred at a time. Multiple births can be risky because they are more likely to be associated with miscarriage, gestational diabetes, pregnancy-related high blood pressure and pre-eclampsia, anemia, and the need for a cesarean section. IVF may also increase the risk for ectopic pregnancy, which means the embryo implants in a fallopian tube rather than in the uterus.
The IVF process can also be taxing and challenging emotionally. Going through IVF can affect several aspects of life, including social connections, romantic relationships, work, finances, and more. The first treatment cycle specifically has been shown to cause higher levels of anxiety and stress.
Alternatives to IVF
Because of the significant emotional, physical, and financial stress associated with IVF, many people may choose to explore alternative routes to pregnancy.
.webp)
Historically, much of the conversation around family-forming benefits has been on IVF, but in reality, less than 3% of infertility cases require invasive treatments like IVF in order to achieve pregnancy or become parents.
In many cases, an alternative may be more appropriate, less expensive, and more compatible with an individual or couple’s lifestyle. There are various fertility treatments and family-building alternatives available, and finding the right one depends on each person or couple’s unique circumstances, values, and preferences.
Intrauterine insemination (IUI) is a type of artificial insemination that involves washing and concentrating the sperm before placing it directly in the uterus around the time of ovulation. Unlike IVF, fertilization during IUI takes place inside the body. While IUI is less expensive, it has lower success rates than IVF, which is generally recommended for couples who have failed to achieve pregnancy after three IUI cycles.
Oral medication used to induce ovulation are often prescribed to women who are experiencing difficulty with ovulation. These medications can help regulate the menstrual cycle and stimulate the release of mature eggs from the ovaries. Two main types of oral medications commonly used for ovulation induction are Clomid (clomiphene citrate) and Letrozole (Femara). Both medications increase the levels of FSH to stimulate the ovaries to produce eggs causing rising levels of estrogen. High levels of estrogen in turn will promote an LH surge, a key event that triggers ovulation.
Individuals or couples may choose to utilize donor eggs or sperm for a variety of reasons, including poor egg quality, early menopause, problems with the ovaries, the risk of passing on known genetic diseases, and more. Same-sex couples, members of the LGBTQIA+ community, and individuals who do not have partners may also choose to use donor eggs or sperm to achieve pregnancy.
If a woman is unable to carry a pregnancy for any reason, she may choose to seek out a gestational carrier or surrogate who can carry and give birth to a baby. Gestational surrogacy is usually done through IVF and there are two kinds of surrogacy: gestational and traditional. In gestational surrogacy, the carrier of the pregnancy (the surrogate) does not provide an egg for fertilization and is therefore not genetically related to the fetus. In traditional surrogacy, the surrogate uses her own egg to conceive. This means that the surrogate is also the biological mother of the child. Typically, artificial insemination is used to fertilize the surrogate’s egg with the intended father’s sperm. Traditional surrogacy arrangements can raise legal, emotional, and ethical complexities. For these reasons, traditional surrogacy is less common than gestational surrogacy.
Some individuals or couples may choose adoption as a route to parenthood and others may pursue adoption if IVF is not an option or if they have tried and been unsuccessful with IVF. There are many different kinds of adoption and logistics to consider in the process, but for many, adoption may be the best option.
Coping with the emotional rollercoaster of IVF
The IVF process can be incredibly challenging for individuals and couples on a psychological and emotional level. Research shows that the depression levels in patients with infertility are comparable to patients who have been diagnosed with cancer. It’s important to pay close attention to the areas of people’s infertility journeys that have the potential to trigger mental health issues. In addition to the unpredictability of IVF and its success, the process can contribute to social isolation, relationship strain, financial stress, and more.
Experts recommend preparing for the emotional challenges of IVF by doing as much research and information gathering as possible prior to embarking on the journey, and to cultivate a strong support network. Identifying stress triggers and coping strategies ahead of time may also help reduce discomfort through the process. It is also important to seek out professional psychological help if stress or emotions become overwhelming.
IVF is a complex process that has helped many individuals and couples achieve pregnancy. For many people dealing with fertility issues including advanced maternal age, ovulation problems, male factor infertility, or unexplained infertility, IVF may be a life-changing opportunity. It is also an important option for same-sex couples and single parents by choice who wish to have a genetically related child.
While there are many potential benefits to IVF, it’s also important to understand the potential financial consequences, as well as emotional and physical challenges. Success rates can vary based on several factors, including the woman's age, the quality of the embryos, and the underlying cause of infertility. It's essential for individuals and couples considering IVF to consult with a qualified fertility specialist or reproductive endocrinologist to understand their specific fertility challenges, explore all available options, and make informed decisions about their fertility journey.
Everything you need to know
Get an overview of what medications may be involved in an IVF journey, how they work, and common side effects.
This guide provides practical guidance on how to create a safe and comfortable space for at-home injections.
Understand how each piece of the IVF process contributes to overall costs.
IVF frequently asked questions
How many rounds of IVF are recommended?
The number of recommended rounds of IVF can vary depending on several factors, including the individual's age, overall health, underlying fertility issues, response to treatment, and financial considerations. The decision on how many IVF cycles to pursue is typically made on a case-by-case basis in consultation with a fertility specialist. It often takes several rounds of IVF to achieve pregnancy and research has indicated that about two thirds (65.3%) of patients will be successful after six or more cycles of IVF.
What is the age limit for IVF?
In many countries, there is no legal age limit for IVF treatment, but some clinics may have their own guidelines or restrictions regarding age. IVF success rates are significantly lower for women in their late 40s and beyond, and the likelihood of achieving a successful pregnancy through IVF decreases significantly. For some women, using donor eggs from younger women may be an option to improve success rates.
Can IVF be done with a low sperm count?
Yes. Sperm count is not necessarily indicative of pregnancy success, but it may make it more difficult for couples. IVF may be a good option for couples in which the male partner has a low sperm count when it is combined with ICSI. This involves the direct injection of a single sperm into an egg and increases the likelihood of successful fertilization and embryo development.
Can IVF be done with blocked fallopian tubes?
Yes. There are a number of reasons a woman’s fallopian tubes may be blocked, including endometriosis, fibroids, pelvic inflammatory disease, and more. Through IVF, a fertility specialist can circumvent the fallopian tubes completely and transfer an embryo directly into the uterus.
Is IVF painful?
While every person is different, most individuals do not experience a significant amount of pain during the IVF process. However, pain is subjective, and some people may find IVF more physically uncomfortable than others. Some parts of the process, including medication injections, may be more likely to cause discomfort than others. But the stimulation and egg retrieval generally do not cause intense pain in most people.
How long does the IVF process take?
While every person’s experience is unique, the IVF process generally lasts about four to six weeks from beginning to end. This includes any necessary preparation time, the 8-14 days of ovarian stimulation, the egg retrieval procedure, fertilization, possible transfer, and pregnancy test.
Can I exercise during IVF?
Light physical activity is encouraged through the IVF process if possible, but patients are advised to avoid high-intensity exercises and movements that involve twisting. This is because the ovaries become enlarged during IVF, which can increase the risk of a rare but serious condition called ovarian torsion. Ovarian torsion involves the ovary, and sometimes fallopian tubes, becoming twisted on themselves, cutting off the blood supply. In lieu of strenuous activities, experts generally recommend about 30 minutes a day of low-impact activities like walking and swimming.
What are the chances of having twins or multiples with IVF?
In 2020, about 12.6% of infants conceived through ART were multiples (twins, triplets, or more) compared with 3.2% of all infants in the birth population overall.