You may have heard a friend or health podcaster in midlife refer to HRT and wondered what the acronym stood for. Hormone replacement therapy (HRT) is the medical term for hormone replacement therapy drugs that treat menopause symptoms which occur during perimenopause, menopause, and postmenopausal times. Hormone replacement therapy (HRT) uses prescription or natural hormones to ease menopause symptoms like hot flashes, mood changes, and bone loss. Most menopause symptoms come from fluctuating hormone levels, usually caused by changes in how much estrogen your ovaries are making.
HRT can help replace hormones that aren’t being produced as much during menopause, like estrogen and progesterone. It can also be referred to as menopausal hormone therapy and is available in different forms. It’s the changes in the hormone production that cause many of the uncomfortable menopause symptoms. HRT for menopause can help with menopause symptoms that result from lower hormone levels like hot flashes, night sweats, thinning of bones, and vaginal changes.
Talk to your healthcare provider about symptoms and whether hormone replacement therapy medication would be beneficial for you.
What is Hormone Replacement Therapy (HRT)?
Hormone replacement therapy is a medical treatment used to relieve menopause symptoms with progestin, a type of progesterone, and estrogen. At times, testosterone might be included in hormone replacement therapy drugs discussions, depending on the symptoms one is trying to address and the woman’s health history.
A doctor might recommend HRT to a woman who’s experiencing menopause symptoms that are interfering with her quality of life, in particular, hot flashes, mood changes, fatigue and/or trouble sleeping, irregular periods, brain fog, headaches and more. If menopause symptoms are interfering with a woman’s personal life and work-life considerations, getting early access to HRT can help her find relief, help her miss fewer days of work, feel better in everyday situations, and help with mood and rest.
Menopause is defined as 12 consecutive months without a period – or spotting – and the average age in the U.S. is 52. Perimenopause is the transitional time leading up to menopause and it can be challenging to nail down when it first occurs in women.
Perimenopause typically starts between ages 45 and 55, and symptoms can last a median of 7.4 years but, for some people, those uncomfortable symptoms may persist for as long as 14 to 20 years.
Hormone therapy can help during perimenopause to manage irregular cycles, night sweats, and emotional changes. In general, hormone replacement therapy is considered a safe way to help with perimenopause symptoms and treat menopause symptoms.
It’s important to understand that hormone therapy and perimenopause are highly-studied areas of medicine and many health practitioners will prescribe it to a woman experiencing menopause symptoms for a determined period of time if her personal history and family history dictates it’s a safe treatment option.
Common types of hormone replacement therapy drugs
There are various types of hormone replacement therapy drugs given for different health scenarios and to address women who have various health conditions or previous surgeries. HRT medications deliver estrogen, and sometimes progesterone, through pills, patches, or topical forms to balance hormone levels. There are also options that address hormone therapy and perimenopause symptoms.
Estrogen-only therapy:
Estrogen therapy is a type of hormone replacement treatment that helps ease common menopause symptoms—like hot flashes, night sweats, and vaginal dryness—that happen when estrogen levels drop. It can also help with discomfort during sex caused by these changes. It’s recommended for someone who has undergone a hysterectomy.
Combined estrogen-progesterone therapy
For those with an intact uterus, the hormone replacement therapy often recommended is combined estrogen-progesterone therapy: a combination of estrogen and progestin together to prevent the uterine lining from thickening, a condition called endometrial hyperplasia.
Benefits of hormone therapy in menopause
There are a multitude of benefits of hormone therapy in menopause. Many types of hormone therapy are FDA approved and there are benefits to systemic hormone therapy (those absorbed into the bloodstream) as well as low-dose therapy that’s inserted into the vagina. These are some of the benefits of hormone therapy in menopause:
- You’ll get symptom relief: In general, research and healthcare practitioners find hormone replacement therapy drugs are helpful for lessening hot flashes, resolving sleep issues, reducing mood swings, improving overactive bladder symptoms, and reducing vaginal dryness.
- You may reap long-term benefits: HR therapy can help with bone health by preventing fractures later in life, improve heart protection if you start within 10 years of menopause, lower your risk of developing type 2 diabetes.
- You’ll experience mental health benefits: Starting hormone replacement therapy may reduce feelings of depression in women with low levels of depression going through perimenopause and menopause. Talk to your doctor about how menopause symptoms impact your quality of life and whether hormone therapy combined with healthy lifestyle changes like exercise and stress reduction can help.
Risks and side effects
As with taking any form of medication, there are risks. Some hormone therapy increased risks include breast cancer, strokes, heart attacks, blood clots, and gallbladder disease. But, for most healthy women under 60, HRT benefits outweigh the risks when started near the onset of menopause.
Common myths surrounding HRT therapy
There are a lot of myths around hormone replacement therapy and a lot of women stopped using HRT in the early 2000s after a study came out saying that some women might be at an increased risk of stroke, heart disease, and breast cancer after taking hormone replacement therapy.
However, later reviews found that those results were taken out of context and not accurately interpreted. The study’s methods and data analysis weren’t fully evaluated at the time, which led to widespread misunderstanding about the actual risks of hormone therapy as well as a surge of brands pushing “hormone supplements” to capitalize on the decline of HRT recommendations.
Consult healthcare professionals
Clways talk to your healthcare team about your individual health background and family history to learn more about which hormone replacement therapy medications are best for you and the side effects to be on the lookout for after starting treatment. They might suggest one of the hormone replacement therapy drugs above or point you toward a natural HRT medicine option.
Natural Hormone Replacement Therapy (HRT) options
Natural HRT medicines use plant-based hormones similar to those your body makes, but only FDA-approved versions have proven safety data.
One might consider trying natural hormone replacement therapy options in the form of dietary supplements or natural, over-the-counter hormone creams that claim to help with menopause symptoms. As of October 2025, the FDA doesn’t know if these natural products are deemed “safe,” or “helpful.”
That being said, natural HRT medicine is an exploratory topic in the scientific community and one you might see ads for online or read discussions about. It’s important to discuss any herbal remedies or natural hormone treatments you plan to try with your doctor as some plants can interfere with other medications.
Natural HRT medicine could include some of the following ingredients: ginseng, red clover, black cohosh, angelica, St John's wort, evening primrose oil. Herbal remedies like red clover contain plant-based hormones that can mimic estrogen, and black cohosh is thought to help balance estrogen and progestogen.
Some hormone replacement therapy products called “bioidentical hormones” are compounded pharmaceutical drugs, and are not FDA-approved because they don’t have evidence that they are proven safe. The phrase “bioidentical” is supposed to be an indicator that these treatments are naturally prepared and, thus, safer and more effective than FDA-approved HRT medications. Keep in mind that evidence of these claims is lacking.
Lifestyle and natural alternatives for hormone balance
While it’s great to have a variety of hormone replacement therapy options available, there are plenty of lifestyle changes you can make to try to balance hormones. Here are some that might provide symptom relief:
- Practice stress relief, build strong bones with exercise, eat healthier: These can help improve sleep, mood, and support your body from the inside out.
- Eat a diet with phytoestrogen foods: Some nuts, seeds, soy products and vegetables might provide relief for various menopause symptoms. Consider adding foods with estrogen-like compounds that are derived from plants, like soybeans, legumes (lentils) and flaxseed.
- Consider herbal supplements (black cohosh, red clover): If you’re going to try a menopause supplement (after checking with your doctor), use one that only contains that one ingredient, like black cohosh for hot flash relief. Red clover might help in women who have severe hot flashes and evening primrose oil has been shown in some small studies to decrease the frequency and severity of hot flashes and night sweats.
Always check with your healthcare provider before buying supplements as these are not regulated by the FDA and some herbal products could have negative side effects, especially if you’re taking other medications.
How to choose the right hrt approach
There are a variety of factors to consider when exploring hormone replacement therapy medication which is why it’s so important to talk to your healthcare team about symptoms and their recommendations:
- Health history: Talk to your doctor about your family cancer history, reproductive health, and cardiovascular history. Hormone therapy is generally considered safe for women to take when it’s within 10 years of menopause, or they are under age 60. In most cases, hormone therapy is not recommended for women with breast or uterine cancer, unexplained uterine bleeding, liver disease, a history of blood clots, or cardiovascular disease.
- Talk to your healthcare team about hormone testing: They might recommend blood tests to establish baseline hormone levels, especially if you’re under age 45 and/or you’re possibly going to include testosterone as part of the hormone replacement therapy regimen. A low dose of hormones is usually prescribed at first and it may take a few months for someone to notice improvements in symptoms.
- Consider a natural route: Explore a variety of treatments that can support overall well-being during menopause and perimenopause, including lifestyle and dietary changes, cognitive behavioral therapy (CBT), mindfulness practices, hypnotherapy, and herbal medicine. A virtual menopause care provider can help you on this journey.
- Get support: Carrot’s virtual menopause care makes it easy to connect with a healthcare provide who’s knowledgeable on menopause, get recommendations on symptom management, whether hormone therapy is recommended and support when you need it.
The best HRT plan is personalized based on your symptoms, health history, and treatment goals.
FAQs
What’s the safest form of hormone replacement therapy?
The safest form of hormone replacement therapy is the one a healthcare provider has prescribed based on your individual health history and symptoms. Beyond that, pills or tablets and patches tend to be deemed some of the safest forms of HRT by medical professionals.
What are the risks of HRT during menopause?
The risks of HRT during menopause or hormone therapy and perimenopause are that there’s an increased risk of stroke, uterine cancer, blood clots and breast cancer but most of those risks can be lessened depending on the type of hormone replacement therapy treatment your doctor recommends and factoring one’s health history and age into recommendations.
Can you start hormone therapy during perimenopause?
Yes, you can start hormone therapy during perimenopause under the direction of a healthcare professional who is taking your health history and family history into consideration. Once they’ve determined that the benefits of hormone therapy outweigh risks, a healthcare provider can work with you to explore a multitude of treatment options available and how they can help ease perimenopause symptoms.
What’s the difference between bioidentical and synthetic hormones?
Bioidentical hormones are plant-derived hormones that are structurally identical or chemically similar to those hormones produced by the body. These can include FDA-approved products, like oral progesterone, as well as some compounded bioidentical medications they approved. Compounded drugs made by a pharmacist using a prescription from your healthcare provider are not as well studied and might come with more risks. Synthetic hormones are standard HRT manufactured hormone replacement therapy treatments that are manufactured in a lab and have fixed doses that have been proven effective if they are FDA approved. Progestin is a synthetic form of progesterone that is similar to the hormone made naturally by the body.
Does natural hormone replacement therapy work?
In general, the FDA says that all natural hormones or those classified as bioidentical that they haven’t reviewed aren’t necessarily safe or effective. Just because the word “natural” is in the term doesn’t mean it’s safe or made from nature. Talk to your healthcare provider about the hormone replacement therapy treatments that will be most effective for your symptoms.
Can HRT be combined with herbal or lifestyle treatments?
HRT can be combined with lifestyle modifications, like healthy eating initiatives for weight management and brain health, exercise and strength training to improve bone health and mood, and taking steps to optimize for better sleep at night — changing up one’s sleep environment and bedding to avoiding caffeine and alcohol after certain times of day. While some women say that herbal HRT treatments help them, it’s a topic to discuss with your healthcare provider as the safety and efficacy of many of these haven’t been proven.
Hormone Replacement Therapy drugs can help
You don’t have to white-knuckle it through perimenopause and menopause. Hormone replacement therapy drugs that have been studied and proven effective can greatly help reduce symptoms and improve quality of life during menopause and perimenopause. Think about it: better sleep, fewer mood swings, reduced hot flashes, and improved vaginal health can go a long way to ensuring you feel better throughout the day.
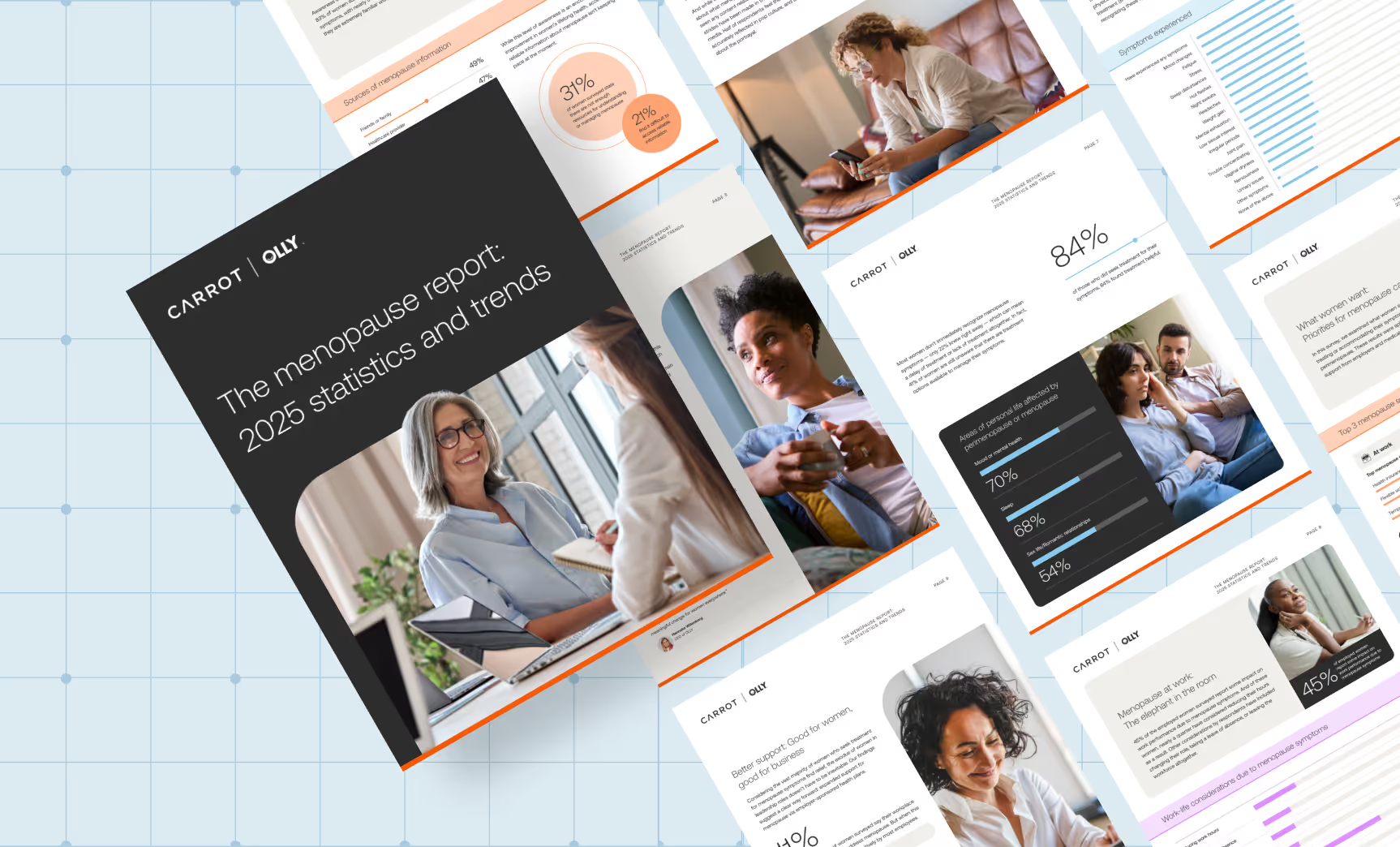
Being educated about HRT is one step to getting relief. In a recent Carrot and Olly study, 44 percent of women surveyed said they are not familiar at all or are not very familiar with HRT as a treatment for menopause symptoms and perimenopause symptoms. In most situations, the benefits of hormonal therapy outweigh the risks for most, so team up with a clinician who can walk you through the possible hormone replacement therapy treatments that would be best for you.
Whether using prescription hormone replacement therapy medication or exploring natural HRT options, the right approach depends on your health needs and preferences.






.jpg)