Intrauterine insemination (IUI) is a fertility treatment that involves placing sperm directly into the uterus after being washed and processed, increasing the number of sperm that reach the fallopian tubes and, subsequently, the chance of fertilization. It’s a less invasive and less expensive fertility treatment option compared to in vitro fertilization (IVF) — a procedure in which eggs, sperm, and embryos are handled outside of the body. IUI is considered a first-line fertility treatment, meaning that couples will generally try IUI before moving to IVF.
Couples may consider IUI if there are issues with sperm quality or quantity or if their infertility diagnosis stems from cervical problems, ovulatory disorders, or endometriosis. It’s also an option for single individuals or same-sex couples wishing to get pregnant.
Explore the blog post:
- Who is a good candidate for IUI
- Benefits of IUI
- Keys to a successful IUI
- The IUI process
- After the procedure
- IUI fertility medications
- IUI success rates
- IUI treatment risks and side effects
- IUI cost
- The bottom line
Who is a good candidate for IUI?
The decision to use IUI isn't limited to a specific group. However, certain circumstances make it an optimal choice for some.
- Unexplained fertility challenges: For starters, IUI may be the first-line treatment for couples experiencing unexplained infertility, mild male factor infertility, ovulatory factor infertility like polycystic ovary syndrome, and uterine or cervical abnormalities, including scarring from past procedures that could impede the sperm's path.
- LGBTQ Community: IUI is frequently an option for lesbian couples wishing to start a family, trans men, and others in the LGBTQ+ community.
- Single parents by choice: Single people using donor sperm, and those for whom intercourse is challenging due to a physical disability or other issues.
It's important to remember that a fertility specialist will consider several factors, including age, overall health, budget, insurance coverage, and specific fertility issues, before recommending IUI or any other fertility treatment.
Benefits of IUI vs. other fertility treatments
When IUI is an option, there can be several distinct advantages over other fertility treatments.
- Less invasive: Unlike IVF, the IUI process is relatively straightforward and less invasive. It does not involve egg retrieval, which requires sedation or anesthesia, making it a less complicated process.
- Cost-effective: Compared to procedures like IVF, IUI is significantly more affordable, making it a viable first step for many individuals or couples facing fertility issues.
- Compatible with donor sperm: IUI allows donor sperm, broadening the possibilities for different types of families, including single individuals and LGBTQ+ couples, to get pregnant.
- Faster treatment cycle: The IUI process is much quicker than IVF and requires fewer doctor visits, potentially leading to less emotional stress and time commitment.
IUI success tips
While it’s more straightforward than IVF, IUI involves physical and emotional preparation. From adopting healthier lifestyle habits to comprehensive medical evaluations, each step you take can contribute significantly to the success of your treatment. Consider the following tips as you plan for fertility treatments:
- Schedule regular medical exams with your fertility specialist. This includes ultrasounds, hormone tests, and semen analysis to check sperm count and motility.
- Consider supplementing with vitamins such as coenzyme Q10. Research published in the International Journal of Molecular Sciences suggests that CoQ10 supplements may help improve egg quality and increase fertilization rates, though more research is needed.
- Learn about the most common IUI medication. Your fertility specialist may prescribe ovulation induction drugs and progesterone supplements to stimulate egg production and prepare the uterus for implantation.
- Eat a balanced diet, exercise regularly, and get enough sleep. A healthy lifestyle facilitates an environment conducive to fertilization. This can look like maintaining a healthy weight, avoiding excessive alcohol use and recreational drugs, and managing stress.
- Seek emotional support. Whether you turn to friends, family, or a therapist, having someone to talk to about the process can alleviate stress.
Medical and fertility evaluations
Your health should be your top priority before and during IUI. Consider the following medical and fertility evaluations:
- Wellness exam: Start with a visit to your obstetrician/gynecologist (OB/GYN), who will conduct a thorough pelvic exam and an overall health check. They will also review your medical history, discuss your fertility goals, and perform basic fertility tests to assess your baseline fertility status.
- Dental exam: Good oral health is crucial when planning for pregnancy. Poor dental hygiene is linked to premature delivery, gestational diabetes, and preeclampsia. Schedule a dental check-up to ensure that your oral health is in optimal condition. Your dentist can treat any cavities or gum disease and provide recommendations on maintaining good oral hygiene throughout pregnancy.
- Fertility consultation: A fertility specialist performs comprehensive fertility evaluations, including an ovarian reserve and hysterosalpingogram (HSG) assessment or a saline infusion sonogram (SIS). The fertility doctor will also coordinate with your OB/GYN to tailor your fertility treatment plan based on your health needs and intended outcome.
Medications and supplements
Your provider may recommend medications and supplements to optimize the chances of successful fertilization. These may include prenatal vitamins with essential nutrients such as folic acid, iron, and calcium. In general, the CDC recommends that all women of reproductive age take 400 micrograms of folic acid a day, in addition to consuming folate-rich foods, such as dark leafy vegetables and whole grains, to prevent birth defects in the baby’s brain. Other supplements may include fish oils rich in omega-3 fatty acids, vitamin D, and CoQ10.
Your fertility specialist may also advise you to take prescription medications throughout the process, such as ovulation induction drugs. These drugs stimulate the ovaries to produce mature eggs and increase the chances of success with IUI.
Timing of IUI procedure
An IUI procedure's timing is critical and carefully coordinated with the menstrual cycle. The process generally starts on the first day of the menstrual cycle. On days two or three, you may be given oral or injectable medications to stimulate follicle growth in the ovaries. Over the next week, your provider will monitor hormone levels and ovarian follicles through ultrasound scans and blood tests.
Once the follicles are an optimal size (around day 13), you may be given a “trigger shot” of a medication known as human chorionic gonadotropin (hCG). The IUI procedure is then scheduled to coincide with ovulation, usually within 24–36 hours after the hCG injection. This precise timing increases the chances of sperm meeting the egg, thereby maximizing the possibility of successful fertilization.
While this is a general timeline, it's important to remember that each individual's cycle can vary, and your provider will determine the exact timing.
Sperm health
Sperm health plays a vital role in achieving successful fertilization. Factors such as sperm count, motility (the ability of the sperm to move efficiently), and morphology (the size and shape of the sperm) can significantly impact the chances of fertilization. A higher number of healthy, motile sperm increases the likelihood of one reaching and fertilizing the egg.
The odds of success with IUI can vary between using known donor sperm and using sperm from a sperm bank. While it might seem that anonymous donor sperm from a sperm bank could offer better quality control, and hence better odds, this is not necessarily the case. The success of IUI relies on many factors, including age, overall health, sperm quality and quantity, and the timing of the procedure. It's always important to discuss these options with your healthcare provider to understand the best route for you.
Before an IUI procedure, sperm undergoes rigorous testing to meet the necessary health standards. This includes an infectious disease screening and a semen analysis to evaluate sperm count, morphology, and motility. Donor sperm also undergoes stringent screening for genetic disorders and infectious diseases like HIV, hepatitis B and C, syphilis, gonorrhea, and chlamydia. These tests are designed to ensure safety and maximize success rates.
Healthy lifestyle
A healthy lifestyle can significantly impact IUI success rates. When your body functions at its best, it can better handle the physical demands of fertility treatment and pregnancy.
- Balanced diet: A nutritious diet is the cornerstone of a healthy lifestyle and is crucial to fertility. Consuming a variety of fruits, vegetables, lean proteins, whole grains, and healthy fats can promote ovulation and improve the overall health of your reproductive system. In addition, certain nutrients such as folic acid, iron, zinc, and vitamins D and C can boost fertility.
- Regular exercise: Regular physical activity can help maintain a healthy weight, regulate hormones, reduce stress, and improve blood flow — all of which enhance fertility health. However, striking the right balance is critical, as excessive exercise can negatively impact fertility.
- Adequate sleep: Lack of quality and sufficient sleep can disrupt the balance of hormones, including those involved in reproduction. Strive for seven to nine hours of sleep per night to ensure your body is well rested.
- Stress management: Elevated stress levels can interfere with fertility. Techniques such as yoga, meditation, or mindfulness can help manage stress and maintain emotional balance throughout IUI.
- No smoking or alcohol: Tobacco, cannabis, and alcohol are linked to fertility complications. Avoid these substances altogether to maximize your success.
- Regular check-ups: Keep up-to-date with routine screenings and health assessments to ensure your body is functioning optimally.
The IUI process
Though relatively straightforward, the IUI procedure is a multi-step process that requires precision and care. Here's a detailed step-by-step guide.
.avif)
1. Preparation of sperm
The first step in the IUI procedure involves preparing the sperm. If using a partner's sperm, the sample is most commonly collected through ejaculation into a sterile container. Semen should be collected after at least 2–5 days of abstinence. If using donor sperm, the sample is thawed in preparation for the procedure. The collected sperm is then "washed" in a laboratory to separate the healthy, motile sperm from the rest of the semen. This process concentrates the most active sperm into a small volume to increase the chances of implantation.
2. Check for ovulation
Before the procedure, you or your provider will confirm ovulation using an over-the-counter ovulation prediction kit, blood test, or ultrasound.
3. The IUI procedure
After lying down on an examination table (similar to a regular pelvic examination), a speculum is inserted into the vagina to enable the doctor to see the cervix.
4. Insertion of the sperm
The prepared sperm is drawn into a syringe fitted with a small, flexible catheter. This catheter is gently threaded through the cervical canal and into the uterus. After injecting the sperm, the catheter and speculum are removed. This process is usually painless, but some people may experience slight discomfort.
5. Post-procedure
Directly after the procedure, you'll remain lying down for 15–30 minutes. There may be a small amount of vaginal discharge or light spotting.
6. Two-week wait
During the two-week period post-IUI, you'll wait to see if the procedure was successful. During this time, your provider may advise you to take progesterone supplements to support a potential pregnancy.
7. Pregnancy test
A blood test is done 14 days after the procedure to check for pregnancy. The test measures beta-human chorionic gonadotropin (hCG) levels in the blood. If the levels are high, it may indicate a successful implantation and pregnancy. If negative, your healthcare provider may suggest a repeat IUI procedure or other fertility treatments.
Pain and discomfort
While the IUI procedure is usually quick and painless, some people may experience mild discomfort (similar to a pap smear) when the catheter is inserted through the cervix. This feeling is temporary and typically subsides within minutes. Mild spotting or cramping immediately following the procedure is also common. However, everyone’s body responds differently. If discomfort persists or if you have any concerns, don’t hesitate to consult your healthcare provider.
What to do after the IUI procedure
Your body doesn't typically require a significant amount of recovery time after IUI. Most people can resume their usual activities after leaving the clinic. However, it may be beneficial to take it easy for the remainder of the day. Some healthcare providers may recommend laying down for up to 30 minutes immediately following the procedure to give the sperm a chance to travel.
During the next two weeks, you may notice symptoms similar to those of early pregnancy or premenstrual syndrome (PMS), such as breast tenderness, bloating, mild cramping, or mood swings. These symptoms are typically due to hormonal changes in your body and could be amplified by the fertility drugs used during treatment. It's essential to understand that these signs are not definitive indicators of pregnancy, and waiting for a pregnancy test is the most reliable way to know the outcome of your IUI procedure.
In addition to physical symptoms, you may feel a mix of emotions, including stress, anxiety, and hope. This two-week waiting period can feel daunting, so it’s important to lean on your support system.
Your healthcare provider will schedule a blood test 14 days after the procedure to check for pregnancy. If the IUI treatment is successful and you become pregnant, you’ll undergo regular prenatal visits to monitor the pregnancy. If the treatment is unsuccessful, your provider will discuss the next steps, which may involve further fertility tests or treatments.
IUI medications
Fertility medications can increase the odds of fertilization with IUI. They stimulate ovulation or increase the number of eggs released during ovulation, enhancing the chances of successful fertilization. The most common medications include:
- Clomiphene Citrate (Clomid or Serophene): This oral medication stimulates the pituitary gland to produce more follicle-stimulating hormone (FSH), leading to the development of one or more mature eggs. It's typically the first choice for inducing ovulation due to its ease of use and minimal side effects.
- Letrozole (Femara®): This oral medication works similarly to Clomid by stimulating the production of FSH but may have fewer side effects for some. It's taken shortly after the start of your menstrual cycle for five consecutive days.
- Human chorionic gonadotropin (hCG): The body naturally produces hCG during pregnancy. An injectable form is sometimes given before or after IUI to induce ovulation of the follicle containing the egg.
- Follicle-stimulating hormone (FSH): FSH is a natural hormone produced by the pituitary gland. Injections of synthetic FSH can stimulate the ovaries to produce multiple eggs simultaneously, enhancing the chances of successful fertilization.
- Progesterone: Your provider may prescribe progesterone supplements to help thicken the endometrium (lining of the uterus) and prepare it for a potential embryo implantation.
- Prenatal vitamins: These are usually recommended before and during pregnancy to ensure that the body has all the essential nutrients.
IUI success rates
There are many factors that contribute to IUI success rates:
- Age
- Overall health
- Cause of fertility challenges
- Timing
- Number of IUI attempts
- Use of medications
- Ovulation regularity
- Sperm quality
Comparing IUI to other fertility treatments can provide a clearer picture of the success rates of assisted reproductive technologies. Getting pregnant through intercourse has a success rate of approximately 20–25% per cycle for healthy couples in their 20s and early 30s, though this rate decreases with age. On the other hand, the success rate of an IUI treatment cycle is around 13% based on a 2021 cohort study published in the Journal of Obstetrics and Gynaecology. IVF success rates are typically higher than IUI, averaging approximately 20% or more per cycle, according to a 2015 JAMA study.
The number of IUI cycles needed depends on individual circumstances and factors, such as age, fertility health, and the cause of infertility. However, 2020 research published in Fertility Research and Practice suggests that the likelihood of achieving a successful pregnancy decreases after three or four attempts. Many doctors recommend moving on to other fertility treatments, such as IVF, after three or four unsuccessful IUI cycles.
IUI treatment side effects and risks
While many experience few adverse effects, others may encounter minor side effects due to the fertility drugs used. Some of the most common include:
- Mild discomfort or cramping
- Temporary spotting
- Mood swings
- Nausea
- Headaches
- Hot flashes
- Breast tenderness
- Fatigue
There are virtually no side effects if an individual undergoes an unmedicated IUI. The potential risks associated with the procedure include:
- Infection: Though extremely rare, there's a small risk of infection after the procedure.
- Multiple pregnancies: Fertility drugs increase the chances of releasing more than one egg during ovulation, which can result in a multiple pregnancy (twins, triplets, etc.). Multiple pregnancies carry higher risks, including premature birth and low birth weight.
- Ovarian hyperstimulation syndrome (OHSS): This is a rare but potentially serious condition caused by an excessive response to fertility drugs. The ovaries become swollen and painful, leading to fluid accumulation that causes rapid weight gain, abdominal pain, vomiting, and shortness of breath.
While these risks and side effects may sound daunting, remember that most people undergo IUI without experiencing any significant problems. Your healthcare provider will monitor your response to treatment closely to minimize any potential risks.
The cost of IUI
The cost of IUI fluctuates greatly depending on your treatment plan, including whether you use fertility medications. An IUI treatment cycle without medication typically costs $300 to $1,200. This cost encompasses the semen analysis, washing of the sperm, and the insemination itself.
The cost can be significantly higher if using fertility medications. While the medication costs vary, they can add an extra $500 to $3,000 per cycle — depending on the type and dosage required. It's important to note that these are average costs. The actual cost can be higher or lower based on the city you're receiving treatment in, the fertility clinic you're using, and your insurance coverage. Your fertility specialist should provide a cost estimate based on your needs.
There are also additional costs for using a sperm donor (IUI-D). The price for obtaining sperm from a sperm bank generally ranges from $300 to $2,000 per vial. You may need more than one vial, especially when undergoing multiple IUI cycles. Shipping and storage fees can add an additional $200 to $500 per shipment.
Is IUI covered under insurance?
Most health insurance plans don't cover fertility treatments, including IUI. However, some states now have laws that mandate fertility treatment coverage for specific groups or individuals. It's worth checking your state's legislation and discussing IUI-related benefits with your insurance provider.
If you don’t have fertility coverage under your health plan, other options are available to help you pay for treatments. Many fertility clinics offer financing plans, low-interest loans, and payment plans to spread the cost over time. Alternatively, some organizations and charities provide grants or other financial assistance to those undergoing fertility treatments.
Some employers offer coverage through fertility benefits like Carrot. If you're interested in speaking with your employer about providing fertility benefits get tips, templates, and other information that can help you approach your HR team.
IUI cost vs. other fertility treatments
Below is a breakdown of the average cost per cycle of common fertility treatments. These costs reflect national averages and can be lower or higher depending on geographical location and individual circumstances.
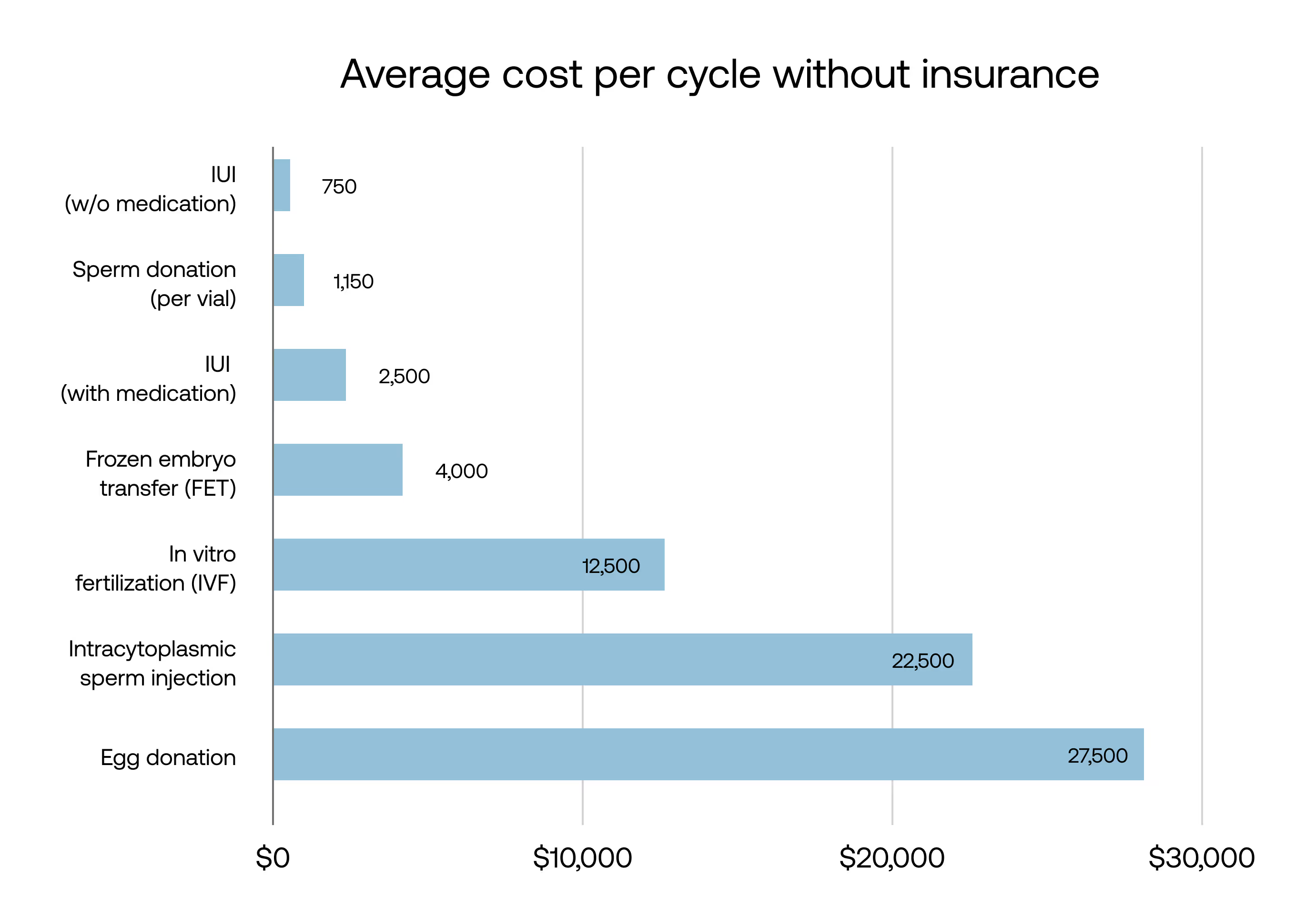
Interested in seeing the cost breakdown of other fertility treatments? Read about the cost of IVF.
The bottom line
IUI has proven successful for many individuals and couples struggling to get pregnant. While the process involves potential risks and side effects, these are typically minor or rare, and the overall procedure is safe and less invasive than other fertility treatments.
The cost of IUI varies significantly depending on whether fertility medications or a sperm donor is necessary, and unfortunately, many insurance plans don’t cover these costs. However, some states mandate coverage under your health plan, and many fertility clinics offer financing options.
At Carrot, we provide comprehensive, inclusive fertility and family-forming benefits that cover a range of fertility treatments, including IUI.













